Sarcomas

The archetypical malignant tumor of fibroblasts, it consists of relatively uniform, mitotically active, tightly packed, elongated cells in a "herringbone" pattern.
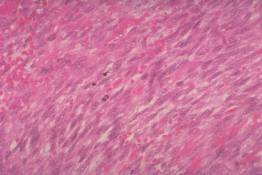
The archetypical malignant tumor of fibroblasts, it consists of relatively uniform, mitotically active, tightly packed, elongated cells in a "herringbone" pattern.
This histologically benign non-metastasizing tumor consists of mature, slow-growing fibroblasts in a collagen rich matrix.
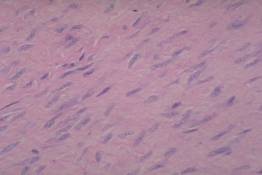
This histologically benign non-metastasizing tumor consists of mature, slow-growing fibroblasts in a collagen rich matrix.

Like fibrosarcomas, MFHs are spindle cell sarcomas but they display much more pleomorphism than do fibrosarcomas. The lineage of the neoplastic cells in this sarcoma has been debated for years. Evidence favors the view that they are bizarre fibroblasts. The low power pattern is more whorled or disorganized than the "herringbone" weave of fibrosarcoma.
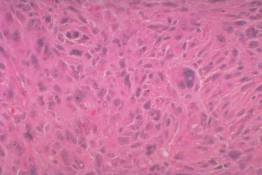
Like fibrosarcomas, MFHs are spindle cell sarcomas but they display much more pleomorphism than do fibrosarcomas. The lineage of the neoplastic cells in this sarcoma has been debated for years. Evidence favors the view that they are bizarre fibroblasts. The low power pattern is more whorled or disorganized than the "herringbone" weave of fibrosarcoma.
The pleomorphic type of liposarcoma, illustrated here, may be confused with MFH. It is identified by neoplastic lipoblasts, tumor cells whose nucleus is dark staining and deformed by developing fat storage droplets in the cytoplasm.
The following case is presented to illustrate how inflammation and repair in connective tissue may be confused with sarcoma. Most errors are due to overcall of benign reactive processes, but this tragic case shows that the error can go either way. All transparencies are made from the original biopsy slides.
A healthy 21 year old man noted a slowly growing lump on the back of his hand, but did not go to a doctor until it became painful. By this time it had been present over a year, and measured 4 cm. in greatest dimension. Surgery revealed a confluent multinodular fibrous mass adherent to tendons. It was dissected free and submitted in pieces for microscopic study. The histologic diagnosis was rheumatoid nodule. Within a few months the mass recurred. When seen again by a different physician a year later, the present mass measured 6 cm and involved carpal-metacarpal joints. Amputation through the forearm was performed. Two months later two pulmonary nodules appeared; he died a few months later.
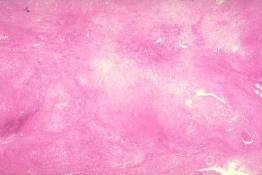
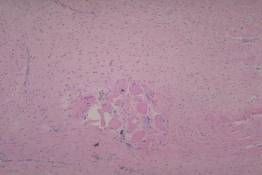
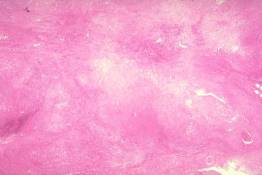
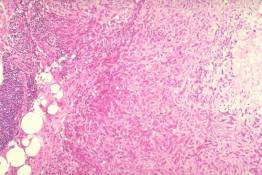
Low power view showing confluent nodules with necrotic centers and inflammatory cell infiltration.
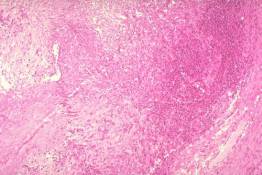
On intermediate power examination, some fields suggest an atypical granuloma with patchy lymphocytic infiltrate.
Other intermediate power fields however, contain cords of atypical cells which raise the question of cancer.
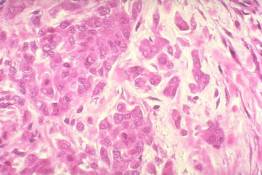
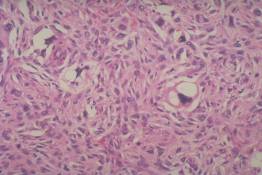
High power examination of a few areas confirms the suspicion of malignancy.
The final diagnosis is epitheloid sarcoma, a rare form of sarcoma containing epithelial elements. It differs from synovial sarcoma (another sarcoma with partial epithelial differentiation) in that it presents clinically as superficial nodules in the distal extremities, and histologically lacks a well defined fibrosarcoma-like component.