Respiratory: URT Tumors
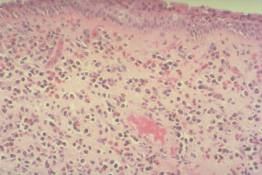
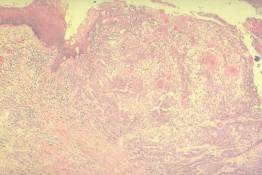
The medium-power microscopic appearance of this lesion is characteristic of a nasal inflammatory polyp. Note the edemetous connective tissue filled with numerous eosinophils (bright pink granules) and plasma cells (blue cells with eccentric round nuclei and perinuclear pink zone in the cytoplasm). The overlying respiratory-type epithelium shows some reactive expansion (hyperplasia) of the basal cell layer but the overlying ciliated epithelial cells are still present.
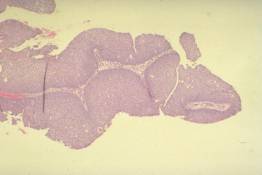
These are finger-like structures that project into the air passages above the surrounding mucosa. They are surfaced by abnormally thick, non-keratinizing stratified squamous epithelium. The epithelial cells are arranged in an orderly pattern and they do not have the cytologic features of malignancy.
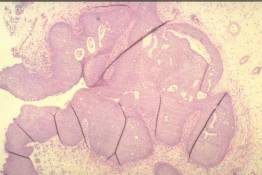
Inverted papillomas and exophytic squamous papillomas are both characterized by proliferations of the same type of epithelium. In inverted papillomas, this epithelium characteristically grows down into preexisting mucosal glands, displacing and replacing the normal epithlium as it proliferates. As the abnormal epithelium continues to expand below the surface, it causes a broad-based mucosal elevation. The epithelium is not cytologically malignant. Although these proliferative lesions often cause local destruction as they expand, the neoplastic epithelium does not actually invade the surrounding connective tissue.
Carcinomas may arise within a preexisting papilloma or directly from non-papillomatous epithelium. All of the epithelial cells here have malignant cytologic features (nuclear enlargement, variability in size and shape) and they are arranged in a disorganized growth pattern. A most important feature is that these abnormal cells have invaded the connective tissue where they infiltrate as small irregular nests and even as individual cells. Contrast this growth pattern with the smooth, expansile epithelial proliferations in the inverted papilloma.
Contrast the normal surface squamous epithelium with that of the adjacent invasive carcinoma. This tumor is classified as a squamous cell carcinoma because some of the tumor cells exhibit recognizable squamous differentiation (note the glassy pink nests of keratinized malignant cells within the tumor). Keratinizing and non-keratinizing squamous cell carcinomas may arise anywhere from the nasal vestibule to the lung as well as inside the oral cavity.
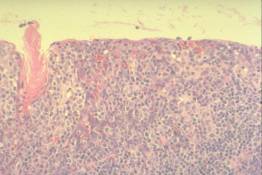
The squamous epithelium of the nasopharynx, tonsils and adenoids (Waldeyer's ring) is specialized to permit lymphocytes to reside within or pass through the epithelium. The thick pink squamous epithelium is almost completely obscured by the small dark blue lymphocytes.
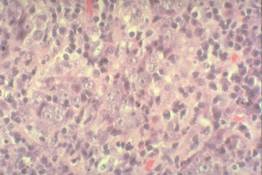
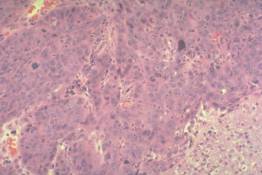
A subset of carcinomas that arise within the nasopharynx retain the ability to interact closely with lymphocytes. This interaction is expressed to a variable extent between tumors but may be so pronounced that the benign (normal) lymphoid cells almost entirely obscure the malignant squamous epithelial cells. Such tumors are sometimes euphemistically described as "lymphoepitheliomas". Metastatic nasopharyngeal carcinomas can be difficult to recognize histologically because the malignant cells are masked by the lymphocytes. Squamous cell carcinomas that lack the tendency to interact with lymphocytes also arise in the nasopharynx.
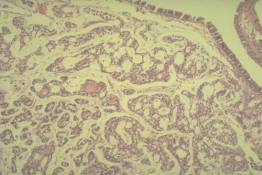
This is the most common type of tumor to arise from the minor salivary glands. The tumor cells are small, have little cytoplasm, and have dark, round to oval nuclei. The cells are arranged as cords, duct-like structures, and larger masses. The larger masses often exhibit a distinctive "cribriform" pattern; i.e. numerous uniform round "cookie cutter-like" spaces are present within the nests of tumor cells. These neoplasms tend to infiltrate widely beneath otherwise normal epithelium and frequently invade nerves.
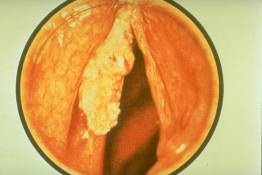
This endoscopic photograph shows a white fungating exophytic mass of carcinoma arising from the right posterior true vocal cord. In addition, the right false cord is thickened and swollen, probably due to infiltrating carcinoma.

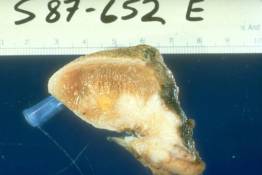
This is a surgically resected larynx and epiglottis with attached left radical neck dissection. The larynx has been opened by making a sagittal incision through the posterior mid-line and a small wooden stick has been inserted to hold the larnyx open. On the right, the vetricle separates the relatively normal false cord (above) from the true cord (below). There is an ulcerated, bloody neoplasm that appears to be centered in the region of the left false cord but the tumor extends transglottically to involve the true cord as well. The radical neck dissection includes the perijugular lymph node chain along with the internal jugular vein and the sternocleidomastoid muscle.

In this clinical photo, the tongue is protruded and elevated to expose the posterior underside where an irregular carcinoma has destroyed part of the tongue. The features that are characteristic of carcinoma include the destructive growth pattern, the variegated color, and disorderly growth. The lesions are also characteristically painless and may bleed.
This is a surgical glossectomy specimen which has been cut in half in the sagittal plane. Only one-half is shown. The tip of the tongue is toward the blue needle hub and the upper surface is nearest the ruler. The white cauliflower-like mass on the underside of the tongue is the invasive carcinoma. It exhibits central necrosis and ulceration. In this case, it extends through the substance of the tongue to within less than 1mm of the surgical margin (which is covered with black ink).